Scifed International Expo on Cardiology-2018
Coronary atherectomy in severely
calcified lesions
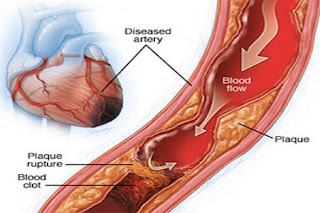
Coronary artery
calcification (CAC) is highly prevalent in
patients with coronary heart disease
(CHD) and is associated with major adverse cardiovascular events. CAC can
usually be found in patients with severe CHD and this asymptomatic phenomenon
make early diagnosis of CAC important. Coronary computed tomographic
angiography is the main noninvasive tool to detect calcified lesions.
Measurement of coronary artery calcification by scoring is a reasonable metric
for cardiovascular risk assessment in asymptomatic adults at intermediate risk.
To date, effective medical treatment of CAC has not been identified. Several
strategies of percutaneous coronary intervention have been applied to CHD
patients with CAC, but with unsatisfactory results. Prognosis of CAC is still a
major problem of CHD patients.
The atherectomy devices that are currently commercially available
differ by design and mechanism of action. The unique mechanisms of action help
to determine which device is best suited for different types of lesions. The
following sections provide an overview of these atherectomy modalities, with a
particular focus on rotational and orbital atherectomy, as they are the two
modalities in current use for severely calcified coronary lesions to facilitate
stent delivery.
Laser atherectomy has been used in the clinical setting since
1983.10 The ELCA
coronary laser atherectomy catheter (Spectranetics Corporation) delivers a
high-energy light beam via a specialized catheter with short pulses, vaporizing
thrombi, and debulking plaque.
Directional coronary atherectomy (DCA) was approved for use
by the US Food and Drug Administration (FDA) in 1990.14 A DCA catheter is equipped with a rotating
cutter that ablates plaque through a small window with the assistance of an
inflated balloon. The rotating cutter is advanced distally, ablating the lesion
and aspirating the debris.
Transluminal extraction catheter (TEC) atherectomy
simultaneously excises and extracts plaque and thrombi15 and received FDA approval in 1993. TEC was
used to treat lesions of heterogeneous morphology and in bypass grafts prior to
angioplasty. TEC is no longer commercially available.
Rotational atherectomy was first used in 1988 and uses
high-speed (140,000–180,000 rpm) rotation to ablate inelastic plaque, resulting
in debris with an average size of < 5 μm.16 Rotational atherectomy has been the most
commonly used atherectomy modality to date. It is commercially available as the
Rot-ablator atherectomy system (Boston Scientific Corporation) and incorporates
a diamond-tipped elliptical burr, which spins concentrically as it advances in
a forward direction.
Cardiology-2018 conference is providing excellent opportunity for the people
related to “Coronary
atherectomy” to meet experts,
exchange information, and strengthen the collaboration among Directors,
Researchers, Associate Professors, and Scholars from both academia and
industry.
For more details, have a glance at PS: http://scientificfederation.com/cardiology-2018/
.png)




0 comments: